Back Pain
If you have lower back pain, you are not alone. About 95% of adults experience lower back pain at some point in their lifetimes.
Most low back pain is acute, or short term, and lasts a few days to a few weeks.
Chronic back pain is defined as pain that persists for 12 weeks or longer. The pain can range in intensity from a dull, constant ache to a sudden, sharp sensation that leaves the person incapacitated.
Basics of Back Pain
“Healthy backs are all alike; every painful back is painful in its own way.” – Dr. Abdollahi.
Pain can be defined as an unpleasant sensory and emotional experience. Pain is subjective. For some patients, back pain is mild. It is bothersome, sometimes flaring up. For other patients, back pain is severe enough to hurt all the time and frequently interrupts sleep.
Back pain can be classified as acute, subacute or chronic.
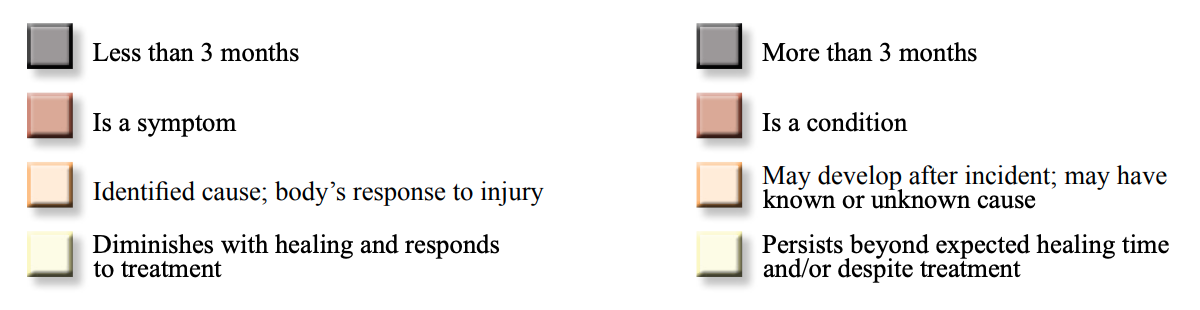
Acute back pain usually lasts from one to several days. About 80% of all back pain is acute.
Subacute back pain usually lasts from several days to several weeks. About 10% to 20% of all back pain is subacute.
Chronic back pain usually lasts more than three months. About 5% to 10% of all back pain is chronic.
Immediate Medical Attention
Most back pain will resolve on its own with time. However, you should see a physician immediately if you experience any of the following:
Back pain that spreads to your legs and extends past the knees
Back pain that results from a fall or injury
Back pain that is accompanied by fever
Back pain that interrupts sleep
Back pain that remains after six weeks
Back pain that causes bowel or bladder problems
Back pain that causes weakness, numbness or tingling in one or both legs
Back pain that is accompanied by unexplained weight loss
Incidence
If you have back pain, you are not alone. Almost 95% of people will experience some form of back pain in their life.
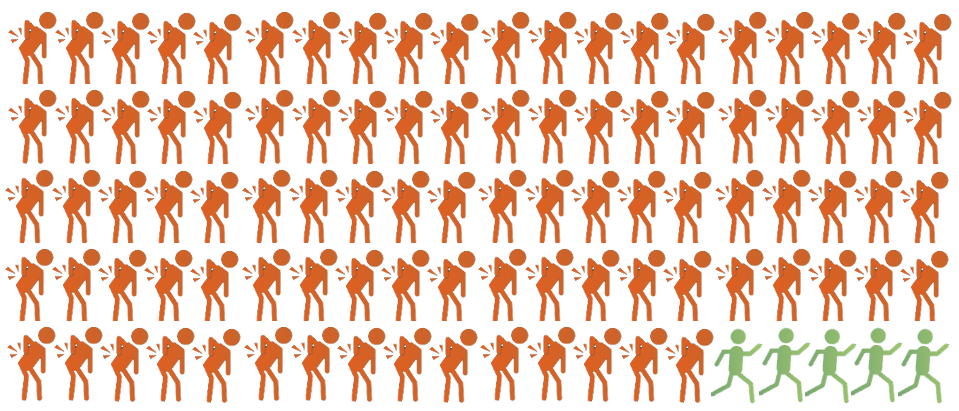
Back pain is the 5th most common cause of visits to a physician. It is the single most common cause of disability worldwide.
Back pain can occur at any age in both men and women. However, it may be more prevalent in women beginning at middle age, due to women’s predisposition to osteoporosis.
Effects of Back Pain
Back pain is one of the leading causes of time lost from work. It can also prevent you from enjoying time with your family and friends.
Back pain is frequently associated with anxiety and depression. It limits physical activities, and the effects on your quality of life can be far-reaching.
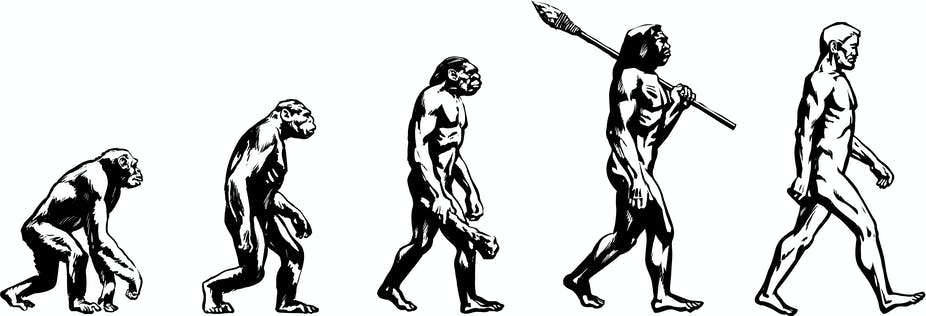
Why Do We Suffer from Back Pain?
The ancestors of humans walked on knuckles and feet. As humans evolved to walk upright, extra stress has been placed on our backs, leading to back pain.
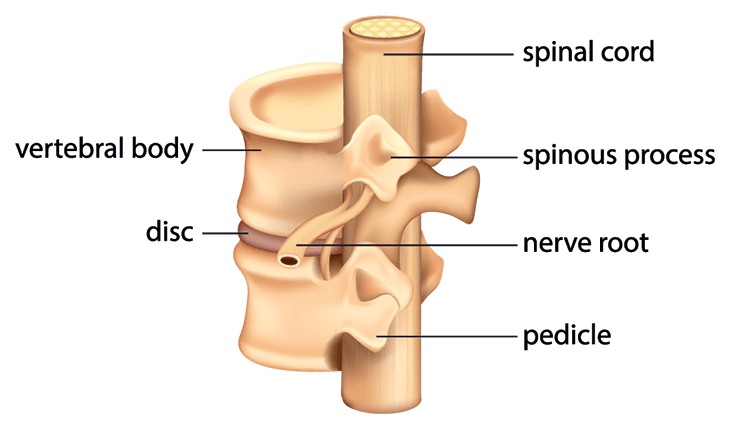
The back is held upright by the spine, consisting of 24 separate vertebrae. These 24 vertebrae are stacked on top of one another. Where two vertebrae meet is called a joint. Joints make it possible for the spine to move and turn in many different directions.
Located between vertebra is a disc made of cartilage. These soft and elastic discs act like cushions that absorb shock, much like shock absorbers in your car. They are crucial in protecting the joints from wearing out.
Running through a hole in the back of each vertebra of the upper and middle spine is the spinal cord. This hole is in the back the vertebra behind where the disc is. If you imagine the spine as a pearl necklace, then the vertebrae are the pearls, and the spinal cord is the string.
The spinal cord transmits signals between the brain and the nerves that run throughout your body. When there is a problem with a part of your body, a signal is generated that works its way to the spinal cord and then to the brain where it is processed as pain.
The spine does not hold the back upright on its own. It requires muscles, tendons, and ligaments for support. Muscles help you move or hold your position. Tendons fasten muscles to bones. Ligaments stretch from one bone to another to hold bones together. There are also backup joints in the back of the spine called facets that help stabilize the back and work like a tripod with the discs.
Causes of Back Pain
As amazing as the human body is, there are also many moving parts that can go wrong. Any condition that puts pressure on your back muscles, joints, discs, or nerves can cause lower back pain. Any illness or damage to your spine also can cause lower back pain. Below are some common causes of back pain.
Osteoporosis
Your body is in a constant state of regenerating the calcium in your bones. One way to think about it is that you are always building new bones and breaking down the old, much like the Golden Gate Bridge is constantly being painted while the elements are wearing down the paint. When you’re young, new bone is made faster than old bones are broken down. As you get older, new bone is created more slowly. The bones that make up your spine become fragile over time. This is called osteoporosis and can lead to loss of height, hunched posture, and back pain.
Fragile bones can break more easily, and there is an increased tendency for this to happen in older women. Osteoporosis also contributes to compression fractures, or spinal fractures in which the vertebrae become flattened. Falls, lifting heavy objects, or moving the wrong way can worsen a compression fracture.
Osteoarthritis
Osteoarthritis is one form of arthritis that can cause back pain. Arthritis is basically inflammation of a joint. Osteoarthritis refers to a specific type that is called degenerative, which essentially means that it is normal wear and tear that happens over time and cannot be reversed. This can also be seen in other major joints like the knees, hips, and shoulders.
In the case of the back, this can happen at the facet joints. Other joints in the back like the sacroiliac joints can also be afflicted.
Osteoarthritis causes a joint to become stiff and lose its elasticity. Over time, the cartilage chips away in certain areas and no longer cushions the joints in the body. If the condition worsens, the bones could rub against each other, causing even more pain and loss of movement. Osteoarthritis can also cause abnormal bone growth that can cause pain.
Osteoarthritis causes muscles, tendons, or ligaments to become strained. Lower back pain can become more intense when osteoarthritis affects the hips or the knees.
Spondylosis
Spondylosis is a general term for age-related wear and tear affecting the spinal disks in your back and neck. As the disks dehydrate and shrink, signs of osteoarthritis develop, including bony projections along the edges of bones (bone spurs).
Facet Arthropathy
Facet joints are small joints located at the back of the vertebrae and as mentioned earlier help stabilize the spine. As you age, your body weight may shift unevenly onto facet joints. This extra burden wears down the cartilage between the facet joints. Without the cartilage to cushion the joints, they rub against each other and become inflamed. In turn, muscles near these facet joints also stiffen and spasm.
Failed Back Surgery Syndrome
Failed back surgery syndrome occurs when patients experience persistent pain after back surgery. Even with a successful surgery, Failed Back Surgery Syndrome is still possible at a rate between 20%-40%.
Injury or accident
Have you ever moved a piece of furniture that didn’t seem too heavy, only to feel pain in your back the next day? Have you ever stretched for something that was just a little out of your reach and felt a twinge in your back? Or maybe you were struggling a little harder than usual pulling a weed while gardening?
Many back injuries are caused by an unexpected twist or sudden motion. The worst offender is trying to work, lift, or perform any other activity while you’re bent forwardly. These activities usually results in muscle spasms, sprains, strains.
Spasms, sprains, and strains all have symptoms such as pain, swelling, and decreased range of motion, but they are each a very different type of injury.
A spasm is an involuntary contraction of muscle. If the spasm becomes chronic, it will shorten the muscle over time, leading to a decreased range of motion and an increased risk for re-injury.
A sprain happens when a ligament is stretched beyond its normal length, which causes a stretching, weakening, or possible tearing of the ligament. Any joint in the body can be sprained, and the most common joint sprained is the ankle.
Whereas a sprain is an overstretched ligament, a strain is an overstretched muscle or tendon. This is most commonly referred to as a ‘pulled’ muscle or tendon.
These injuries usually last 48 to 72 hours, followed by days or weeks of less-severe pain. It usually takes two to four weeks to heal completely from a mild back injury. It could take from 6 to 12 weeks if the injury is more severe. Severe back injury from a fall or accident may require hospitalization and a longer recovery period.
Myofascial tenderness/strain
The fascia is the connective tissue that covers muscles. Myofascial pain syndrome is a broad term for muscle pain. It is characterized by specific sensitive spots known as trigger points. When there is pressure on these trigger points, patients feel pain in a different part of their body. Often people have myofascial pain that feels like sciatica when it is actually and strained or spasmed muscle.
Trigger points
Trigger points are localized spots on the body that produce referred pain. This means that even though the pain is created in one specific location, it can cause pain to be felt in other areas. Trigger points are associated with mysofascial pain syndrome and fibromyalgia.
Nerve entrapment/nerve compression
Nerve entrapment or nerve compression is a medical syndrome that develops when nerves become compressed (or entrapped) and restricted. This occurs due to a variety of causes, from trauma or injury to repeated or overuse activity.
Ruptured intervertebral disc
Imagine a pearl necklace again. Now imagine one of the beads popping out and straining the string inside. A ruptured or herniated disc acts similarly when it bulges into the spinal canal, pressing on the nerve roots. A disc can rupture after bending over and lifting, or it may occur for no apparent reason.
A ruptured disc may cause back pain and muscle spasms, but a more common symptom is sciatic pain. This is severe pain spreading down one leg and often into the foot. It can also be associated with numbness and tingling. But remember, myofascial pain can also cause this same shooting pain sensation. Also, many people with no pain at all often have bulging disks and have no symptoms at all.
Spinal stenosis
Imagine the pearl necklace where the holes in the beads are so tiny that they pinch the string inside. In spinal stenosis, the spinal canal becomes narrowed. This squeezes the spinal cord and nerves running in the spinal canal. This pressure can cause back pain. Numbness, pain and weakness in the legs can also occur. The most common symptom of spinal stenosis is pain that worsens when walking or standing and subsides when sitting down or bending forward.
Ankylosing Spondylitis
Ankylosing spondylitis is a form of arthritis that causes the joints in the spine to become stiff and swollen. It most often affects the lowest areas of the spine and can be associated with autoimmune disorders. In time, stiff joints can fuse and grow together. The most common symptoms are pain and stiffness in the buttocks and lower back that continue for more than three months.
Rheumatoid Arthritis
Rheumatoid arthritis causes any joint to become stiff, painful and swollen. It can affect the neck but almost never the joints in the lower back.
Polymyalgia Rheumatica (PMR)
Polymyalgia Rheumatica is a rheumatic disorder that causes muscle pain, aching and stiffness in the neck and shoulders, lower back, thighs and hips. It can last a few months or many years. Most people experience severe stiffness in the morning.
Fibromyalgia
People with fibromyalgia feel pain and stiffness in muscles and tendons, especially in the neck and upper back. The pain can last for weeks, months or years. The symptoms may disappear by themselves. This condition often is related to sleep problems, poor conditioning or an old injury.
Paget’s Disease
Paget’s disease is a type of disorder in which the calcium in the bone spreads unevenly. The bones most commonly affected are in the lower back, pelvis, tailbone, skull and long bones of the legs. Back pain may be a symptom, but most often there are no obvious symptoms. Paget’s disease usually is discovered on an X-ray or bone scan done for reasons other than pain.
Other Conditions that Cause Back Pain
Sometimes pain felt in the back actually originates elsewhere in the body. Such problems may include:
-
Prostate trouble in men
-
Problems with reproductive organs in women
-
Kidney diseases, such as an infection or kidney stone
-
Diseases of the intestines or pancreas, such as cancer or a blockage cancer that has spread to the spine
-
Multiple myeloma, a form of cancer of the bone and bone marrow
-
Abnormal curving of the spine such as scoliosis or kyphosis
-
Rarely, a tumor on the spinal cord
Diagnosis of Back Pain
Your doctor will take a thorough history, extensive physical exam, potentially order imaging, and sometimes order lab work. Regardless of what type of doctor you see, there are some things you can expect your doctor to do during your visit. Your doctor first will ask you a number of questions, the most common of which are listed as follows:
-
What are your exact symptoms?
-
Where is the pain?
-
When did the pain begin?
-
How long have you had the pain?
-
Did a specific accident or injury cause your back pain?
-
What improves the pain?
-
What makes the pain worse?
-
Have you noticed any other symptoms or changes since the pain began?
-
What treatments have you tried?
-
Do you have any other health problems?
-
What kind of work do you do?
-
In what types of recreational activities do you participate?
Next, your doctor will perform a physical exam. During the exam, the doctor may inspect your muscles and joints. He may ask you to sit or lie down or ask you to move your back in different positions. This is to evaluate your range of motion. He will check the area of most pain and see if other areas of your body are tender or painful. Reflexes, muscle strength, and sensation will also be evaluated.
Diagnostic Tests
If the doctor needs more specific information, he or she may ask you to undergo one or more of the following tests to identify the likely cause of your pain:
X-ray
In certain cases, X-rays might indicate that pain is due to: injury in one or more of the back bones, a tumor in the spine, or a deformity in the spine.
CT Scan
Some people with lower back pain may need a CT scan. A special machine takes multiple X-rays of the area, and a computer converts this scan into a three-dimensional view of the back. A doctor will be able to see if there is a ruptured disc, spinal stenosis, or an infection of the spinal cord that can’t be seen on regular X-rays.
Electrodiagnostic Studies
Electrodiagnostic studies are used to help confirm the presence of nerve compression in the spine. An electrodiagnostic study consists of two tests. One is an electrical test, which is designed to study nerve conduction. In this test the nerve is given an electrical stimulation, and the speed of the impulse is measured. The other test is a needle test called an electromyogram, or EMG. The purpose of this test is to study the muscles for primary disease or for the effect of nerve compression on the muscle. It can also identify potential issues with nerves in the arms and legs that can help to make a stronger case for the pain either coming or not coming from the spine. The compression is especially seen in herniated discs or spinal stenosis.
MRI
MRI (magnetic resonance imaging) is another way to make very clear pictures of parts of the spine. The MRI does not use X-rays or radioactive dyes. It uses a large magnet that produces a strong magnetic field that forces protons in the body to align with that field. It can provide clearer pictures of soft tissues such as muscles, cartilage, ligaments, tendons and blood vessels, in addition to bone structure.
Myleogram
During a myelogram, a special liquid dye called contrast medium is injected into the spinal canal. X-rays are then taken of the area. The contrast medium can make problem areas show up more clearly on the x-ray. A doctor may order a myelogram to detect problems such as spinal stenosis or spinal cord tumors. If surgery is being considered, particularly for a person who has had a serious back injury, many neurosurgeons will require a myelogram beforehand.
Bone Scan
During a bone scan, a very small amount of radioactive liquid is injected into a vein and concentrates in the bones for a short time. A special radioactive detecting machine will scan the area of concern to produce a picture. Occasionally bone scans are done to look for damage or tumors in the bones themselves. However, back pain is rarely due to diseases of the bones.
Blood Tests
If your doctor orders blood tests for you, a laboratory technician will carefully draw a small amount of blood from a vein in your arm, which then will be tested in the laboratory. Ask for an explanation of the tests.
More than 85 percent of people with lower back pain improve with minimal treatment in a matter of days. However, if back problems persist, we (back pain doctors near me) take a multi-modal approach to managing your pain.
Injections
A variety of injections are are available that can help relieve back pain. The needle can be placed in muscles, near an affected nerve, or in and around joints. Depending on the type of pain, various anesthetic or anti-inflammatory medications will be delivered through the needle at the targeted locations. Sometimes, a specialized needle will be used to deliver radiofrequency heat to destroy the nerve and reduce your back pain.
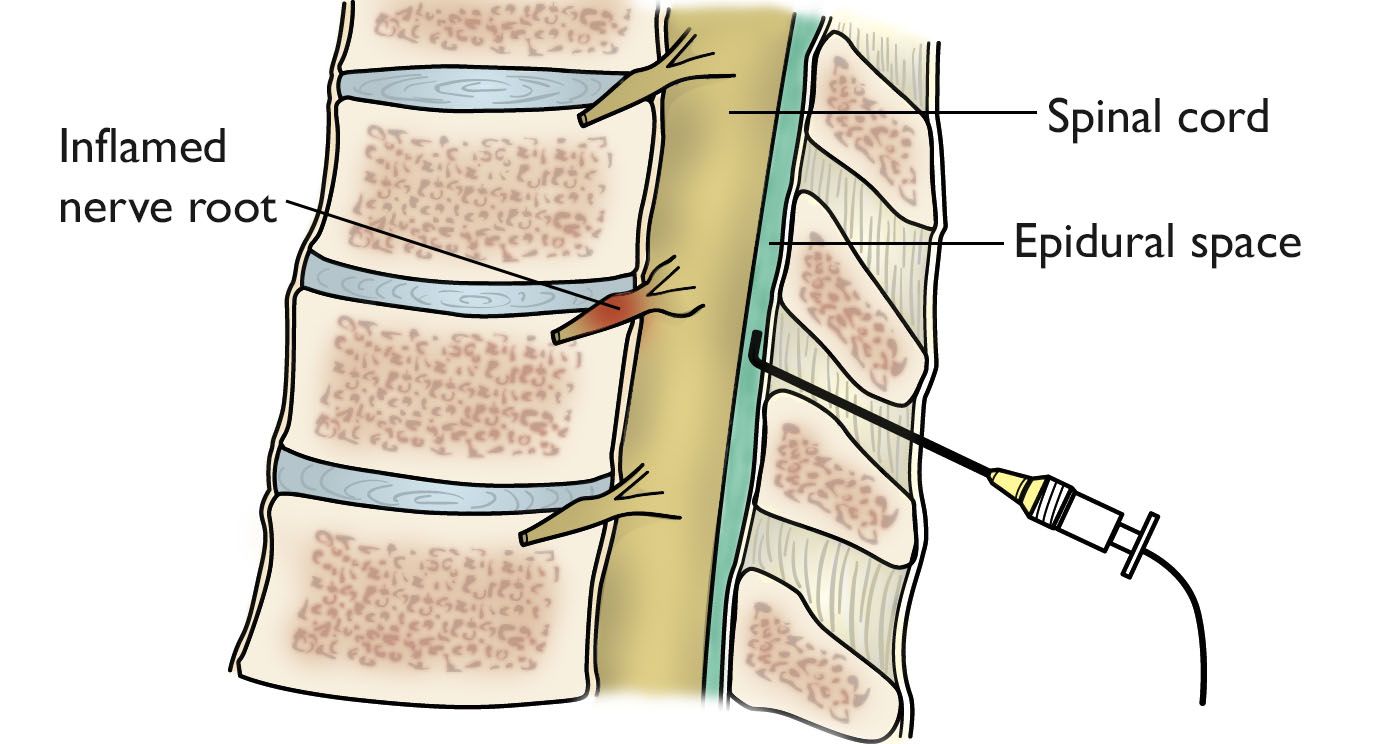
Epidural Injection
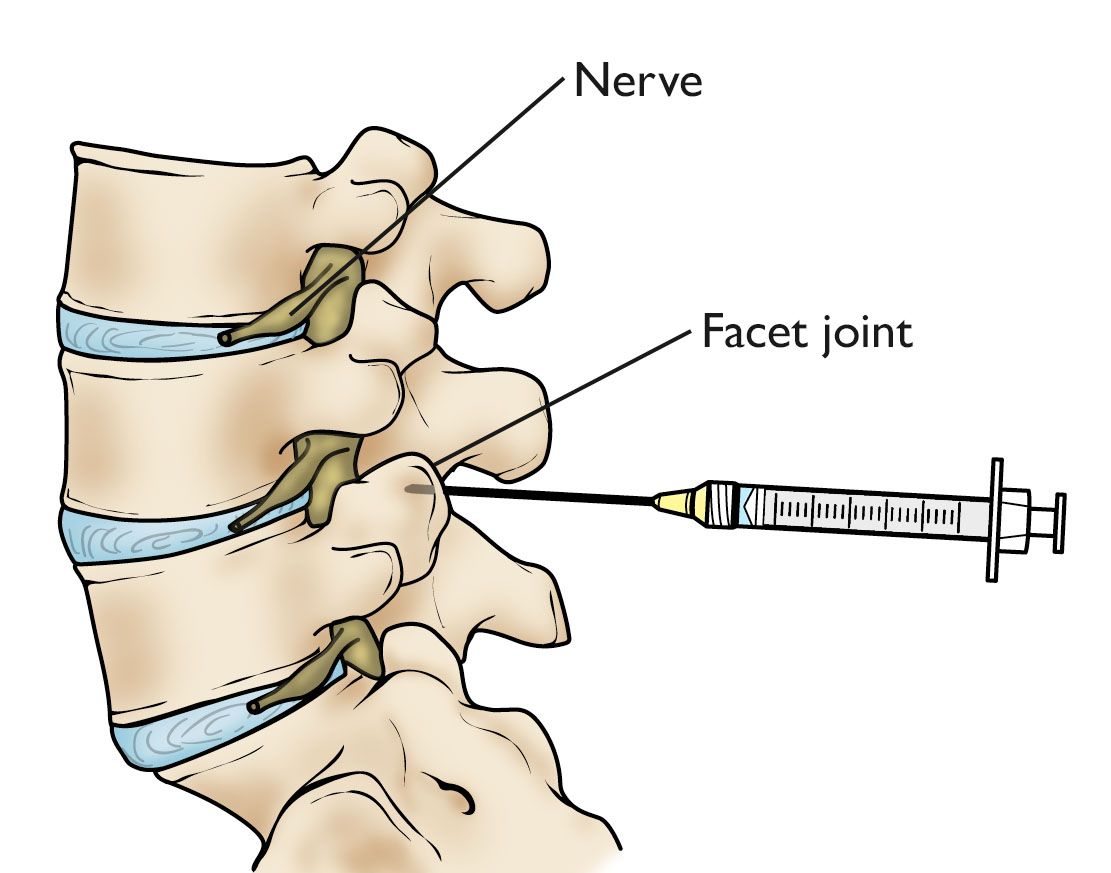
Facet Joint Injection
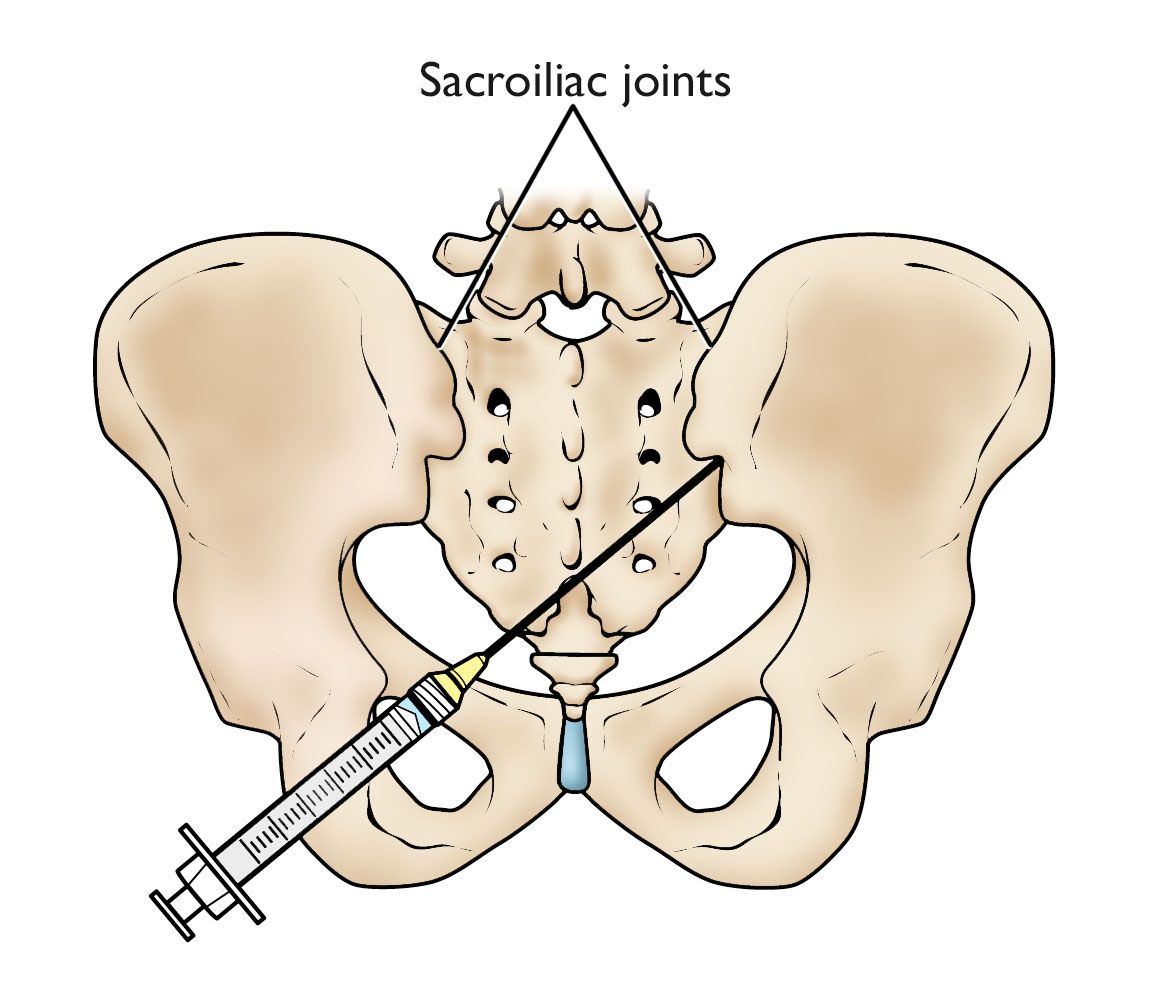
Sacroiliac Joint Injection
Minimally-Invasive Procedures for Back Pain
The field of pain medicine is evolving rapidly. Thanks to technology, there are many more options today to treat your pain. California Advanced Pain & Spine Specialists is committed to using the latest technology to help you reclaim your life.

Intrathecal Pumps
Intrathecal pump is a method of giving medication directly to your spinal cord. A round metal device about the size of a hockey puck is surgically placed under the skin of your abdomen. A small plastic tube is connected to the pump and delivers medication to the area around your spinal cord.
The pump slowly and consistently releases medication over a period of time. It can be programmed to release different amounts of medication at different times of the day, depending on your changing needs. When the reservoir is empty, Dr. Salazar simply refills the pump. This procedure is completely reversible if you ever decide to have the pump removed.
Intrathecal pumps work more efficiently than oral medication. In fact, your symptoms can be controlled with 1/300 the amount of medication than when taken orally. Less medication, fewer side effects.
We (doctors for back pain near me) currently manage over 600 intrathecal drug delivery devices.

Stimwave Therapy
Stimwave therapy uses a wireless and fully programmable device to deliver stimulation to your nerves to treat pain at its source. The device is placed with a needle next to the target nerves. You control the stimulation with a Wearable Antenna that can be clipped to your clothing. The stimulation can be programmed to personalize your pain relief on your cell phone.
Stimwave therapy can target pain anywhere on your body. With Stimwave therapy, you can experience relief from your pain, decreased medication usage, and an improved quality of life.

Spinal Cord Stimulator
Spinal Cord Stimulator
Spinal cord stimulator interrupts pain signals before they reach the brain. SCS systems have a stimulator and thin wires that are implanted into your body. The stimulator delivers tiny pulses of mild electric current through the wires to specific nerves on the spinal cord. These impulses mask pain signals traveling to the brain.
A remote control allows you to turn stimulation on and off, increase and decrease the level of stimulation, and target different pain areas in your body using settings or programs designed specifically for you. Spinal cord stimulator systems can reduce your pain by more than 50%.
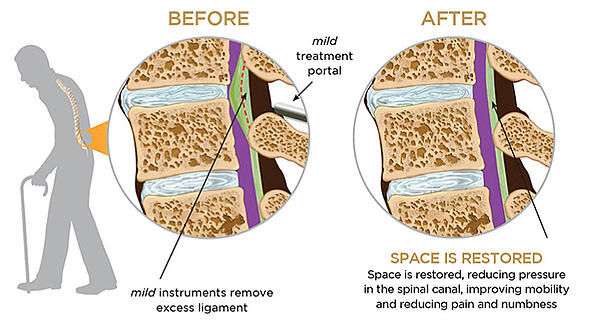
mild® Procedure by Vertos
The mild® procedure treats neurological claudication which involves a narrowing of the lower spinal canal that causes pain in the lower back, legs or buttocks. During the mild® procedure, a doctor will remove small pieces of bone and excess ligament tissue through a tiny incision in the back to restore space in the spinal canal. It is a short, outpatient procedure, performed through a very small incision (about the size of a baby aspirin) that requires no general anesthesia, no implants, and no stitches. Study data show that 79% of patients experience a significant reduction in pain and significant increase in mobility.

Indirect Decompression by Vertiflex
As we age, the shape and size of our spinal canals change. This sometimes cause compressing of the nerves traveling through the lower back into the legs and results in pain. Indirect decompression involves introducing a small implant into the patient’s spine, which relieves pressure on the affected nerves and reduces pain.
Medications
If your back pain is not relieved using other forms of treatment, your doctor may prescribe medications. The medication chosen depends on the your specific symptoms and the cause of your back pain. Analgesics can help relieve pain. Muscle relaxants can help relax tight muscles. NSAIDs (or non-steroidal anti-inflammatories) can reduce inflammation and pain caused by inflammation. Neuropathic medications help reduce pain thats caused by injured or damaged nerves. Various biologic medications are available to treat autoimmune and rheumatological disorders.
If you are taking opioids for chronic pain, be careful of a phenomenon called opioid-induced hyperalgesia. Long-term use of opioids can actually increase your sensitivity to pain. In these cases, intrathecal pumps can help.
Surgery
Patients with sciatica or spinal stenosis often benefit from surgery. However, most people can be treated successfully with rest, exercise, minimally-invasive procedures, and medication.
Psychotherapy and Pain Psychology
If stress is making your back pain worse, a mental health professional specializing in pain psychology may help. At California Advanced Pain & Spine Specialists, a specialist in pain psychology will help you can identify stressors that worsen your pain. They can teach you how to handle your stress. They can help you manage the effect of back pain on your life. You can also talk to them about any emotional issues as a result of pain.
Working with a pain psychotherapist, you are able to gain techniques to focus your mind and thoughts in a way to take control over your pain.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy is a highly effective method of pain psychology. CBT helps individuals resolve their problems concerning maladaptive emotions, behaviors, and cognitions through a goal-oriented, systematic process. While it was originally used for treatment of those with depression and anxiety disorders, it has been shown to be highly effective in treating pain.
Biofeedback
Biofeedback involves gaining greater awareness of physiological functions such as muscle tone, skin conduction, heart rate, or brainwaves. Information on a specific process is gathered, amplified, and displayed (fed back) to the patient who then uses the visual or auditory feedback to gain control over the targeted behavior. Biofeedback has been used to treat a variety of chronic back pain.
Acupuncture
Acupuncture involves the insertion of needles into acupuncture points in the skin in an effort to relieve pain. Although the mechanism for acupuncture remains unclear, studies have shown acupuncture produces physiologic effects that are relevant to analgesia.
Physical Therapy
Reduction in bodily movement that can be related to fear of pain or re-injury is common in back pain and often leads to physical deconditioning and, subsequently, increased pain. Physical therapy is an integral part of chronic pain interventions as it helps restore physical functioning and reengagement in rewarding life activities. Physical therapy involves a range of activities including stretching exercises, strengthening exercises, and use of graded exercise techniques such as therapeutic pools or stationary bikes, in addition to a range of palliative therapies such as spinal manipulation and ultrasound, among others.
Back Pain Relief
No matter how severe your back pain is, there can be things you can do at home to ameliorate the pain. Please consult your physician for specific medical advice.
Diet
Imagine wearing a 25 lb backpack every day, every minute, every second. How strained would your back be? These extra pounds are what an overweight person carries all the time everyday regardless of what they are doing. Don’t be surprised (or offended) if your doctor recommends weight loss as one way to reduce your back pain and improve your general health. The best way to lose weight is with a balanced diet along with regular exercise. Everyone can do some form of exercise. The best diet is the right diet for you. Be sure to avoid fads or unrealistic regimens.
Exercise
The key to a healthy back is proper exercise. Some exercises are designed to strengthen your back and core muscles, while other exercises are designed to improve your posture. 30 minutes of aerobic exercise three times a week is ideal for overall fitness. Walking and water exercise are highly recommended for most people with back problems. The right kind of exercise can not only keep your back problem under control, but it can make doing your daily activities easier. Always consult your doctor before beginning any exercises. It has been shown that exercise is the best way to treat myofascial pain which happens to be the most frequent cause of back pain.
Rest
Rest from strenuous work or other activities is a frequently recommended treatment for acute back pain. But remember that exercise (not rest) is recommended for subacute and chronic back pain. Depending on the severity of your acute back pain, different amount of rest will be needed. Usually, two to three days of staying away from strenuous activities will be enough to ease your back pain. This again takes into account that far and away most back pain is short lived and often caused by myofascial strains and sprains.
Hot and cold treatments
Many people have found that hot and cold treatments help relieve back pain. You might try both to find out which works better for you. Heat relaxes muscles, soothes painful areas, and helps bring in blood flow to the area. Cold numbs muscles, relieves pain, and helps avoid blood flow that can cause inflammation and pain. Ice is often the better initial choice.
To apply heat:
-
Take a hot bath
-
Use a hot water bottle or heating pad
-
Use a heat lamp
To apply cold:
-
Use an ice bag or a package of frozen peas
-
Massage area with an ice cub
Posture training
If poor posture is a factor, then posture training may help relieve your back pain. Ask your doctor about posture training, during which you will be taught healthier ways to sit, stand, sleep, and lift.
Techniques for good posture
When sitting:
-
Sit in a firm chair with armrests to relieve pressure in your back and shoulders.
-
Keep your upper back straight and shoulders relaxed. Keep stomach muscles pulled in, and maintain the proper curve in your lower back. You can do this by tightening your stomach and buttocks. Some people are more comfortable sitting with the back of the chair at a 15- to 20-degree angle.
-
Use a small cushion behind the lower back to maintain the natural curve of the back.
-
Place a footstool under your feet to keep your knees slightly higher than your hips.
-
Stretch every now and then.
When standing:
-
Stand with weight equally distributed on both feet.
-
Don’t lock your knees.
-
Place one foot on a footstool to ease tension in your back.
-
Keep your back straight by tightening your stomach muscles and buttocks.
-
Focus on bringing your scapulas in towards each other with your chest stretch out
When sleeping:
-
Lie on your side with your knees bent.
-
If more comfortable, place a pillow between your knees while sleeping on your side.
-
Use a firm mattress.
Body mechanics
It is important to keep good posture while your body is in motion. When you lift, hold the object close to the body and lift with your legs. This maintains the normal curve of your back and prevents uneven pressure on the vertebrae of your spine.
When bending down to lift an object, bend with your knees instead of your back. Avoid bending forward to lift or work.
-
Hold the object close to you.
-
Straighten your legs to lift the object.
-
Get help with an object that is too heavy.
Back pain may be common, but you don’t have to suffer. Everyone’s pain is different and requires a different treatment plan.
Pain management physicians are specialists with a high level of training in the diagnosis and treatment of different types of pain. They have usually completed 4 years of medical school, 4 years of residency, and 1 year of pain management fellowship before they can treat your pain. Frequently, they will attend conferences and seminars that teach the latest innovations in pain treatments as the field of pain management evolves in complexity.
Relieving pain is not about just taking medications but involves physical, behavioral, and psychological therapies for the best results. The goal of pain management is exactly what it says: to manage pain. No one can always be without pain, but by using all the tools available the goal is to reduce the pain (and pain perception) to a level that allows you to take part in the activities you enjoy and improve your quality of life.
California Advanced Pain & Spine Specialists takes a multi-modal approach to treating pain. Whether it is with simple injections, more advanced technologies (spinal cord stimulation, intrathecal pumps, peripheral nerve stimulation), medications, psychotherapy, or various combinations of all of the above, our physicians will develop an individualized treatment plan for your pain. We will take care of you and do everything possible to get you back to enjoying your life.





Robert G. Salazar MD
Dr. Salazar was born and raised in Corcoran, California. He is the sixth of eight children born in a Spanish-speaking farmworker family. This instilled work ethic at an early age.
He graduated from Stanford with a degree in Human Biology and received his Doctorate of Medicine from the University of Southern California in 1979.
The following year, Dr. Salazar completed an internship at Los Angeles County – USC Medical Center in Internal Medicine.

Alireza Abdollahi-Fard MD
Dr. Abdollahi-Fard enjoys an active lifestyle reaching back to his participation in high school basketball and volleyball teams. As a result, he has had his share of injuries and knows firsthand the frustration of chronic pain.
He has always strived to show special empathy towards patients who are often allowed very little respite from their debilitating symptoms.
Dr. Abdollahi-Fard sees pain as the only chronic medical condition where the patient is acutely aware of, and affected by the disease
Let Us Help You

